01.05.12
For 5 days at the end of April, in L’viv and Kyiv, a series of seminars, presentations and conferences were held to help palliative care grow in Ukraine.
Palliative care is a comprehensive approach to providing the best possible quality of life for terminally ill patients and their families by offering adequate pain management through early and accurate diagnosis, appropriate treatment methods and psycho-social and moral support.
According to current international approaches and concepts, palliative care should be an inalienable and integral part of health and social care. The 1990 WHO Declaration and the 1996 Barcelona Declaration call on all countries to include palliative care as part of their national health care systems. The British colleagues who came to Ukraine stress this fact and are eager and happy to help develop palliative care in Ukraine.
Due to the difficulty of obtaining narcotic analgesics, 80% of terminally ill patients suffer unnecessarily in Ukraine; patients  in the villages have the hardest time obtaining effective analgesics.
in the villages have the hardest time obtaining effective analgesics.
Official death statistics in Ukraine show that every year a minimum of 80,000 cancer patients suffer unnecessary pain. This figure doesn’t include others, such as those living with HIV, TB and other diseases who also suffer from acute or chronic pain.
Doctors are unable to help in these cases because they are unable to get access to narcotic analgesics, it notes in a Human Rights Watch report which investigated the basic approaches to palliative care in Ukraine. “There is no reason why a person should be forced to live out their final months suffering. Even overwhelming pain can be controlled. 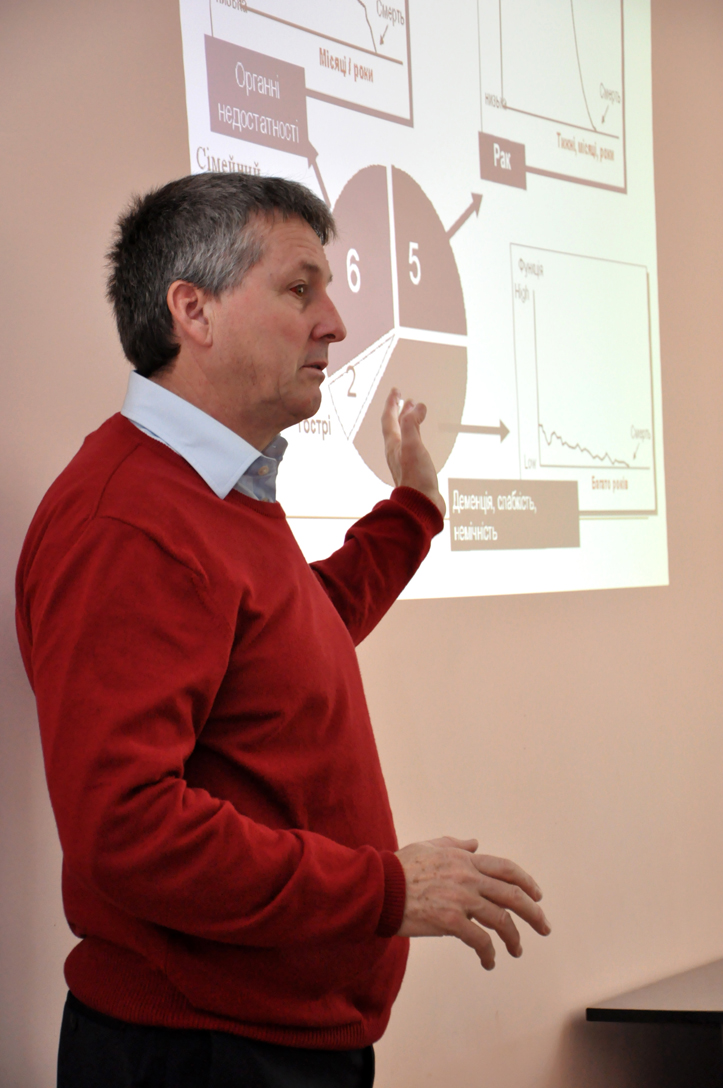
Ukraine just has to develop adequate laws to address the use of narcotic medicines,” said Diedrick Lohman, Senior Health Researcher for Human Rights Watch.
The international organization notes that oral morphine is forbidden in Ukraine despite being identified by the WHO as one of the most indispensible medicines in treating the terminally ill. In Ukraine, temporary pain relief that morphine affords can only be obtained by injection; however for this to be effective, a patient needs to receive injections 6 times a day. A license to keep morphine is only issued to central district hospitals; village inhabitants obviously have a difficult time getting to these establishments, note human rights observers. This situation could be resolved if a suitable number of Hospices functioned in the country whose function is to treat the terminally ill; however there are very few of them. Currently there are only 9 stationary hospices in the country and 10 palliative care units housed in regular hospitals. These establishments can serve up to 650 individuals, but the minimal need is 3000 note experts.
During a recent visit made by British colleagues to Ukraine—representatives of medical and religious establishments—a slew of specialized public events f or doctors, spiritual leaders, students and other interested individuals were held on the topic. They also participated in meetings with leaders of medical establishments and officials. The organizers of these events were Caritas Ukraine and the Churches’ Regional Commission in North East England.
or doctors, spiritual leaders, students and other interested individuals were held on the topic. They also participated in meetings with leaders of medical establishments and officials. The organizers of these events were Caritas Ukraine and the Churches’ Regional Commission in North East England.
A meeting held on 25 April in L’viv, in the conference hall of the Andrey Sheptytsky Hospital, organized by Caritas Ukraine, presented research conducted by Sister Yosafata (Oksana Dobryk) entitled Palliative Care as a way to Prevent Euthanasia.
At an open seminar on 26 April in Kyiv, representatives from the League of Palliative Care, the International Renaissance Foundation, government officials, and medical personnel met. “To unite the efforts of everyone, to activate the local and professional communities and medical establishments—this is the assignment we are giving ourselves,” said Dzvenyslava Chaykivs’ka, the m eeting’s organizer. “The Ukrainian government must finally recognize the wisdom of subsidiarity and allow appropriate social services and palliative care to be delegated. They also must ensure access to narcotic analgesics.
eeting’s organizer. “The Ukrainian government must finally recognize the wisdom of subsidiarity and allow appropriate social services and palliative care to be delegated. They also must ensure access to narcotic analgesics.
I hope that the British experience and their models of palliative care will become the norm for everyone in their final days, not only a dream for those who were lucky enough to hear about it during events—I hope it puts a mechanism in motion that will develop and strengthen our palliative care system.”
Tags: